RFK Jr.’s New Vaccine Panel Sparks Debate: Will It Reshape Childhood Immunization?
6/26/20255 min read
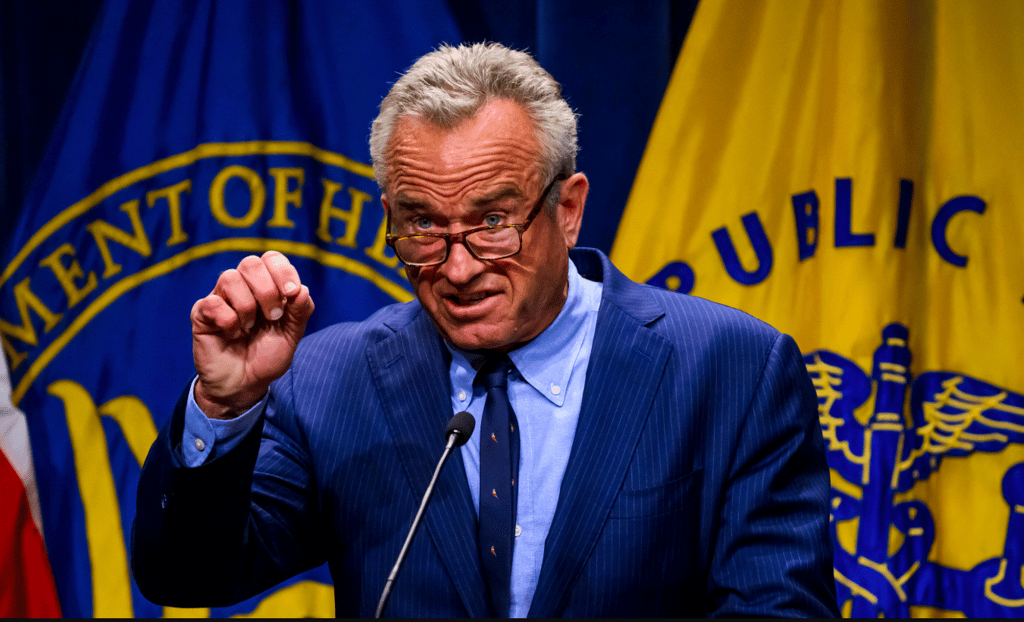
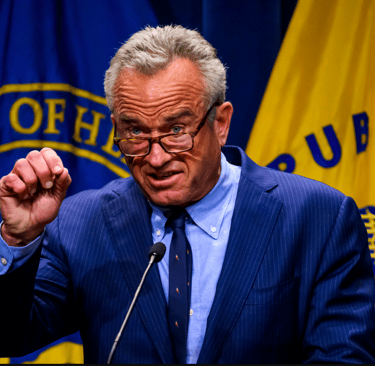
RFK Jr.’s New Vaccine Panel Sparks Debate: Will It Reshape Childhood Immunization?
Introduction: A New Chapter for U.S. Vaccine Policy
On June 25, 2025, the Advisory Committee on Immunization Practices (ACIP) convened its first meeting with a completely new roster at the Centers for Disease Control and Prevention (CDC) headquarters in Atlanta. Handpicked by U.S. Health and Human Services Secretary Robert F. Kennedy Jr., this panel is tasked with scrutinizing the childhood vaccine schedule—a move that has ignited both hope and concern across the nation. With Kennedy’s history of vaccine skepticism, the public is watching closely to see how this overhaul might impact immunization policies that affect millions of American children. In this post, we’ll explore the implications of this shakeup, the new panel’s priorities, and what it could mean for public health.
What Happened: A Clean Sweep of ACIP
In a bold and unprecedented move, Kennedy dismissed all 17 previous ACIP members on June 9, 2025, citing concerns over conflicts of interest and a lack of rigorous vaccine safety scrutiny. Just two days later, he announced eight new members, many of whom have expressed skepticism about certain vaccines or past public health policies. The new panel includes figures like Dr. Robert Malone, a vocal critic of mRNA vaccines, and Vicky Pebsworth, linked to the National Vaccine Information Center, a group known for questioning vaccine safety. Other appointees, such as Dr. Cody Meissner and Dr. Martin Kulldorff, bring academic credentials but also controversial stances on issues like COVID-19 policies.
The ACIP, established in 1964, plays a critical role in shaping U.S. vaccine policy. Its recommendations determine which vaccines are included in the childhood immunization schedule, influence insurance coverage, and guide the Vaccines for Children program, which provides free shots to millions of low-income kids. With this new roster, the panel is set to revisit long-standing vaccine protocols, starting with the hepatitis B shot given at birth and the use of thimerosal, a mercury-based preservative removed from most childhood vaccines since 2001.
Why It Matters: Trust, Science, and Public Health
Kennedy’s decision stems from his stated goal to restore public trust in vaccine science. In a Wall Street Journal op-ed, he argued that the previous ACIP was a “rubber stamp” for industry interests, plagued by conflicts of interest. He claims the new panel will prioritize “evidence-based medicine” and “gold-standard science,” demanding rigorous safety and efficacy data before making recommendations. Supporters, like Mary Holland of Children’s Health Defense, praise the move as a step toward “honest science.” They argue that questioning the vaccine schedule could address public concerns about the rising number of recommended childhood vaccines, which has grown from three in 1986 to over 70 doses by age 18 today.
However, critics warn that this overhaul could undermine decades of public health progress. Dr. Richard Besser, former acting CDC director, called the move “horrifying,” arguing it destabilizes a trusted system that has saved countless lives. The American Medical Association and Infectious Diseases Society of America have also voiced concerns, noting that the new panel’s lack of deep vaccine expertise could lead to recommendations that fuel vaccine hesitancy. With measles cases nearing a decades-high and whooping cough on the rise, some fear that weakening trust in vaccines could exacerbate outbreaks of preventable diseases.
The Panel’s Priorities: What’s on the Table?
At its June 25-26 meeting, the ACIP signaled plans to dive into several contentious issues:
Cumulative Effects of Childhood Vaccines: The new chair emphasized analyzing the combined impact of multiple vaccines given to children, a concern often raised by vaccine skeptics who question whether the current schedule overwhelms young immune systems.
Hepatitis B Vaccine at Birth: The panel will scrutinize the safety and necessity of administering this vaccine to newborns, a practice standard since the 1990s to prevent chronic liver disease.
Thimerosal in Vaccines: Despite its removal from most childhood vaccines, the panel will revisit thimerosal’s safety, with a presentation by Lyn Redwood, a former leader of Children’s Health Defense. Critics argue this focus revives debunked claims linking thimerosal to autism.
COVID-19 and Other Vaccines: The agenda includes discussions on COVID-19, HPV, RSV, and meningococcal vaccines, raising concerns that established recommendations could be scaled back.
These priorities reflect Kennedy’s longstanding focus on vaccine safety, but they’ve sparked alarm among experts who say the science behind these vaccines is already robust. For example, thimerosal’s safety has been affirmed by dozens of studies, and the hepatitis B vaccine has drastically reduced infection rates.
The Controversy: Expertise vs. Ideology
The new ACIP’s composition has drawn sharp criticism. While some members, like Dr. Meissner, have prior ACIP experience, others lack current expertise in vaccinology. Dr. Malone, for instance, has suggested without evidence that COVID vaccines cause cancer, while Retsef Levi has claimed they harm young people. Dr. Sean O’Leary of the American Academy of Pediatrics likened the panel’s overhaul to replacing air traffic controllers with novices who doubt aviation. Critics argue that the rushed vetting process—completed in just two weeks compared to the usual months—raises questions about the panel’s impartiality and qualifications.
On the other hand, Kennedy’s supporters argue that the previous ACIP was too cozy with pharmaceutical companies, pointing to a 2009 HHS report that noted disclosure “omissions” by members. The new panel, they say, brings fresh perspectives and a commitment to transparency. David Mansdoerfer, a former HHS official, called the shakeup a “huge win for the medical freedom movement.”
Potential Impacts: Access, Coverage, and Public Trust
The ACIP’s recommendations have far-reaching consequences. If the panel scales back the vaccine schedule, insurers might stop covering certain shots, making them cost-prohibitive for some families. The Vaccines for Children program, which serves about half of U.S. kids, could also be affected, creating inequities in access. Dr. Walter Orenstein, a former CDC immunization director, warned that reduced recommendations could deter vaccine manufacturers from investing in the U.S. market, potentially limiting supply.
Public trust is another concern. The ACIP’s rigorous, transparent process has long been a global model for vaccine policy. Critics fear that a panel perceived as anti-vaccine could erode confidence, especially amid declining childhood vaccination rates. However, Kennedy’s supporters argue that addressing public skepticism head-on could rebuild trust by showing that vaccines are being thoroughly re-evaluated.
What’s Next: A Pivotal Moment
The ACIP’s June meeting is just the beginning. With only eight members, the panel lacks a quorum for voting, meaning ex-officio members from other HHS agencies may need to step in. The absence of a permanent CDC director—Kennedy has been making final recommendations himself—adds another layer of uncertainty. Meanwhile, Congress is pushing back, with the House Committee on Oversight and Government Reform demanding details on the dismissals by June 24.
As the panel digs into the vaccine schedule, its decisions could reshape how Americans access and perceive vaccines. Will it strengthen public confidence through transparency, or will it fuel skepticism and reduce immunization rates? Only time will tell, but the stakes are high.
Thought-Provoking Questions for Readers
Do you think a fresh perspective on vaccine safety could rebuild public trust, or does it risk undermining established science?
How should the government balance transparency with maintaining confidence in proven public health measures?
What role should public skepticism play in shaping vaccine policy, and how can experts address legitimate concerns without fueling misinformation?
hello@boncopia.com
+13286036419
© 2025. All rights reserved.